Introduction to Heart Failure
Heart failure is a serious and complex condition that affects the way your heart pumps blood throughout your body. As an experienced human writer, I understand the importance of providing a comprehensive and visually appealing guide to help you better understand this condition. In this article, we’ll explore the causes, symptoms, types, diagnosis, and treatment options for heart failure, as well as lifestyle changes and tips for living with this condition.
Causes and Risk Factors of Heart Failure
Heart failure can be caused by a variety of factors, including:
- Coronary artery disease: This is the most common cause of heart failure, as it can damage the heart muscle and impair its ability to pump blood effectively.
- High blood pressure: Uncontrolled high blood pressure can put a strain on the heart, leading to heart failure over time.
- Heart valve problems: Issues with the heart’s valves, such as stenosis or regurgitation, can make it harder for the heart to pump blood efficiently.
- Cardiomyopathy: This is a disease of the heart muscle that can be inherited or caused by factors like alcohol abuse or certain medications.
- Congenital heart defects: Some people are born with structural problems in their heart that can contribute to heart failure.
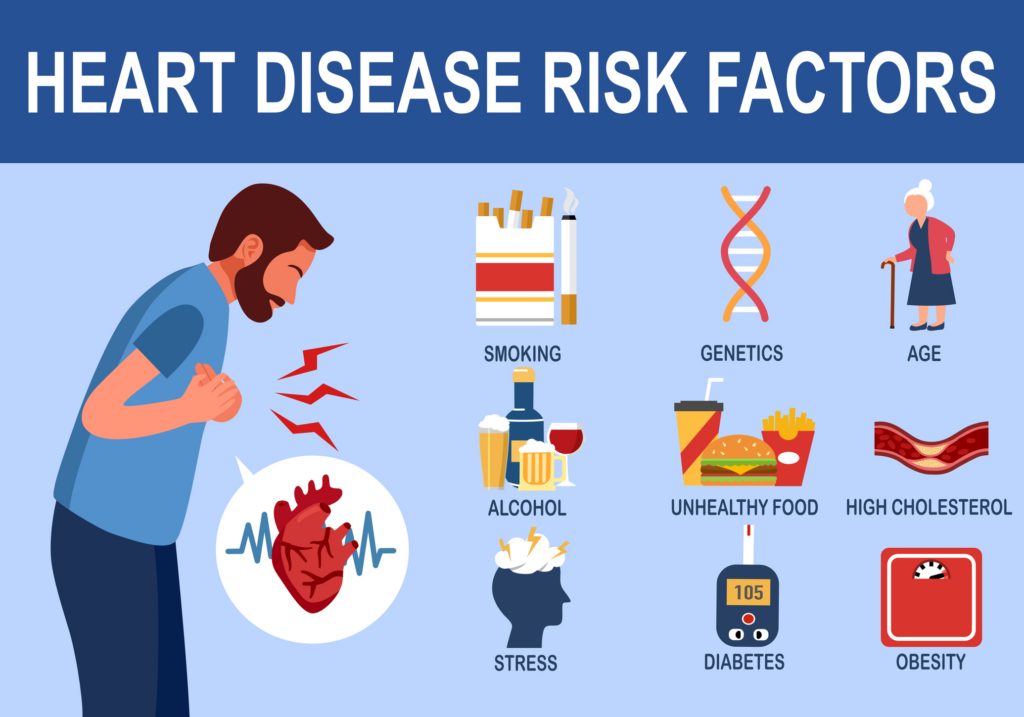
Certain risk factors can also increase your chances of developing heart failure, such as:
- Age: The risk of heart failure increases as you get older.
- Diabetes: High blood sugar levels can damage the heart and blood vessels.
- Obesity: Being overweight or obese puts additional strain on the heart.
- Smoking: Smoking can damage the heart and blood vessels, leading to heart failure.
Signs and Symptoms of Heart Failure
The signs and symptoms of heart failure can vary depending on the type and severity of the condition. Some common symptoms include:
- Shortness of breath, especially during physical activity or when lying down
- Fatigue and weakness
- Swelling in the legs, ankles, and feet
- Persistent cough or wheezing
- Lack of appetite, nausea, or a feeling of fullness
- Confusion, memory loss, or impaired thinking
- Irregular or rapid heartbeat
It’s important to pay attention to these symptoms and seek medical attention if you experience any of them, as early detection and treatment can greatly improve the outlook for someone with heart failure.
Read More:
Heart Failure: A Comprehensive Visual Guide to the Condition
Types and Stages of Heart Failure
There are several different types of heart failure, each with its own unique characteristics:
- Systolic heart failure: This is the most common type, where the heart’s ability to pump blood is impaired.
- Diastolic heart failure: In this type, the heart has difficulty filling with blood during the relaxation phase.
- Right-sided heart failure: This occurs when the right side of the heart is unable to pump blood effectively to the lungs.
- Left-sided heart failure: This is when the left side of the heart is unable to pump blood effectively to the rest of the body.
Heart failure is also classified into stages based on the severity of the condition:
- Stage A: You are at risk of developing heart failure, but you don’t have any symptoms yet.
- Stage B: You have structural heart disease, but you haven’t experienced any symptoms of heart failure.
- Stage C: You have current or past symptoms of heart failure.
- Stage D: You have severe, persistent symptoms of heart failure that require specialized treatment.
Understanding the type and stage of your heart failure is important for determining the most appropriate treatment plan.
Diagnosis of Heart Failure
Diagnosing heart failure typically involves a combination of the following:
- Medical history and physical examination: Your healthcare provider will ask about your symptoms and any underlying health conditions.
- Blood tests: These can help identify biomarkers that may indicate heart failure or rule out other possible causes of your symptoms.
- Imaging tests: Procedures like echocardiograms, cardiac MRIs, and chest X-rays can provide detailed information about the structure and function of your heart.
- Stress tests: These evaluate how your heart responds to physical activity or stress, which can help identify any underlying issues.
- Cardiac catheterization: This invasive procedure involves inserting a thin, flexible tube into a blood vessel and threading it to your heart to measure pressures and assess blood flow.
Based on the results of these tests, your healthcare provider can determine the type and stage of your heart failure and develop an appropriate treatment plan.
Treatment Options for Heart Failure
The treatment for heart failure can vary depending on the underlying cause, type, and severity of the condition. Common treatment options include:
- Medications: Various types of medications, such as diuretics, ACE inhibitors, and beta-blockers, can help manage symptoms and improve heart function.
- Devices: Implantable devices like pacemakers, defibrillators, and cardiac resynchronization therapy (CRT) devices can help regulate the heart’s rhythm and improve pumping ability.
- Surgery: In some cases, surgical interventions like valve repair or replacement, coronary artery bypass grafting, or heart transplantation may be necessary to address the underlying cause of heart failure.
- Lifestyle changes: Adopting a healthier lifestyle, such as following a low-sodium diet, exercising regularly, and managing stress, can also play a significant role in managing heart failure.
Your healthcare provider will work with you to develop a personalized treatment plan that addresses your specific needs and goals.
Lifestyle Changes to Manage Heart Failure
Making certain lifestyle changes can be an important part of managing heart failure. Some key recommendations include:
- Dietary modifications: Limiting your intake of sodium, saturated fats, and added sugars can help reduce the strain on your heart and improve your overall health.
- Regular exercise: Engaging in moderate physical activity, such as brisk walking, swimming, or light resistance training, can help improve your cardiovascular fitness and overall well-being.
- Stress management: Finding healthy ways to cope with stress, such as through meditation, yoga, or counseling, can help reduce the burden on your heart.
- Tobacco cessation: Quitting smoking and avoiding secondhand smoke can significantly improve your heart health and reduce your risk of complications.
- Weight management: Maintaining a healthy weight or losing excess weight can ease the demands on your heart and improve its function.
- Medication adherence: Consistently taking your prescribed medications as directed is crucial for managing your heart failure and preventing complications.
By incorporating these lifestyle changes into your daily routine, you can play an active role in managing your heart failure and improving your overall quality of life.
Tips for Living with Heart Failure
Living with heart failure can be challenging, but there are strategies you can use to maintain your health and well-being:
- Educate yourself: Understand your condition, the treatment plan, and the importance of following your healthcare provider’s recommendations.
- Communicate with your healthcare team: Regularly discuss your symptoms, concerns, and any changes in your condition with your healthcare provider.
- Monitor your symptoms: Keep track of any changes in your symptoms, such as shortness of breath, swelling, or fatigue, and report them to your healthcare provider.
- Maintain a healthy lifestyle: Adhere to your dietary, exercise, and stress management routines to support your heart health.
- Seek support: Engage with support groups, counselors, or loved ones to help you cope with the emotional and practical challenges of living with heart failure.
- Be prepared: Develop an emergency plan in case your symptoms worsen, and know when to seek immediate medical attention.
- Stay positive: Maintain a positive outlook and focus on the aspects of your life that you can control to improve your overall well-being.
By following these tips and working closely with your healthcare team, you can take an active role in managing your heart failure and maintaining the best possible quality of life.
Complications and Potential Outcomes of Heart Failure
Heart failure, if left untreated or not properly managed, can lead to a variety of complications, including:
- Arrhythmias: Irregular heartbeats can occur, which can be life-threatening if not properly treated.
- Kidney damage: Heart failure can impair the kidneys’ ability to function, leading to additional health problems.
- Liver damage: The liver may be affected by the decreased blood flow caused by heart failure.
- Fluid buildup: Excess fluid can accumulate in the lungs, abdomen, and extremities, causing further complications.
- Stroke: Heart failure increases the risk of blood clots forming, which can lead to a stroke.
The potential outcomes of heart failure can vary widely, depending on the underlying cause, the severity of the condition, and the effectiveness of the treatment. Some individuals with well-managed heart failure may have a relatively good prognosis and be able to maintain a good quality of life. However, in more severe cases, heart failure can be a life-threatening condition.
Conclusion: Importance of Early Detection and Management of Heart Failure
Early detection and proper management of heart failure are crucial for improving outcomes and quality of life. By understanding the causes, symptoms, and treatment options for this condition, you can take an active role in your healthcare and work closely with your medical team to develop an effective plan for managing your heart failure.If you or a loved one are experiencing symptoms of heart failure, don’t hesitate to speak with a healthcare professional. Early diagnosis and treatment can make a significant difference in managing this condition and improving your overall health. Schedule an appointment with a cardiologist today to learn more about the personalized care and support available to you.

